This patient education piece is designed to help improve patients’ understanding regarding rectal prolapse, specifically its presentation, evaluation and treatment. This information may also be useful to the friends, families, and caregivers of patients dealing with rectal prolapse.
Treatment of this condition may often require surgery, and this patient education material is intended for patients with rectal prolapse who are considering or have been recommended surgery. It will address why surgery may have been recommended, what the various treatment options are, what it involves and how it may help patients.
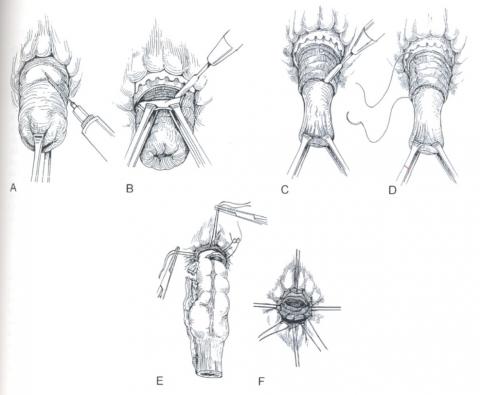
Rectal prolapse is a condition in which the rectum (the last part of the large intestine before it exits the anus) loses its normal attachments inside the body, allowing it to telescope out through the anus, thereby turning it “inside out”. While this may be uncomfortable, it rarely results in an emergent medical problem. However, it can be quite embarrassing and often has a significant negative impact on patients’ quality of life.
Although an operation is not always needed, the definitive treatment of rectal prolapse requires surgery.
While a number of factors have been shown to be associated with rectal prolapse development, there is no clear cut “cause” of rectal prolapse. Chronic constipation (infrequent stools or severe straining) is present in 30-67% of patients, while an additional 15% experience diarrhea. Some have assumed that the development of rectal prolapse is a consequence of multiple vaginal deliveries; however, up to 35% of patients with rectal prolapse have never had children.
Rectal prolapse tends to present gradually. Initially, the prolapse comes down with a bowel movement (BM) and then returns to its normal position. Patients may later describe a mass or “something falling out” that they may have to push back in following a BM. Until the prolapsed rectum goes back in, patients may feel like they are “sitting on a ball”. Rectal prolapse may be confused with significant hemorrhoid disease and can even be confusing at times to physicians not frequently evaluating and treating this problem.
Removal of colorectal polyps is advised because there is no test to determine if one will turn into cancer. Nearly all polyps can be removed or eliminated during a colonoscopy. Large polyps may require more than one treatment. Rarely, some patients may require surgery for complete removal.
Once a colorectal polyp is completely removed, it rarely comes back. However, at least 30% of patients will develop new polyps after removal. For this reason, your physician will advise follow-up testing to look for new polyps. This is usually done 3 to 5 years after polyp removal. Taking a daily aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs) may reduce the risk of new polyps forming. If you had polyps removed, ask your physician if you should take this medication to help prevent them from coming back.